Neurological disorders are becoming one of the most pressing healthcare challenges worldwide. Among them, Parkinson’s disease stands out due to its progressive nature and complex diagnosis process. Traditional clinical diagnosis depends heavily on motor symptoms, which often appear after significant neurological damage has already occurred.
This is where Detecting Parkinson’s Disease using artificial intelligence and machine learning is transforming healthcare.
Advancements in data science, predictive analytics, and biomedical engineering are enabling earlier identification of subtle signs. These technologies are reshaping the way neurologists assess risk, diagnose patients, and plan interventions.
Understanding Parkinson’s Disease
Parkinson’s disease is a neurodegenerative disorder that primarily affects movement. It results from the loss of dopamine-producing neurons in the brain.
Common symptoms include:
- Tremors
- Muscle rigidity
- Slowed movement
- Postural instability
- Speech changes
- Writing difficulty
According to the World Health Organization, millions of individuals worldwide live with Parkinson’s disease. Early diagnosis can significantly improve quality of life.
Why Early Detection Matters
By the time motor symptoms appear, nearly sixty percent of dopamine neurons may already be damaged. Early identification enables:
- Timely medication
- Better symptom management
- Lifestyle interventions
- Slowed disease progression
Detecting Parkinson’s Disease in its early stages improves long-term clinical outcomes and reduces healthcare burden.
Detecting Parkinson’s Disease with AI and Machine Learning
Artificial intelligence systems analyze patterns in patient data that may not be visible to clinicians.
AI models use:
- Voice recordings
- Handwriting samples
- Gait patterns
- Brain imaging scans
- Sensor data
Machine learning algorithms identify correlations between subtle biomarkers and disease progression.
This shift from reactive to predictive healthcare is revolutionary.
Data Sources Used in Parkinson’s Prediction
Several datasets support research in this field.
Common data types include:
Voice Data:
Changes in speech frequency, jitter, shimmer, and pitch variation.
Gait Data:
Stride length, walking symmetry, and movement irregularities.
Imaging Data:
MRI scans analyzed using deep learning.
Biomarker Data:
Protein levels and genetic markers.
Real-Time Clinical Examples
Example One: Voice Analysis
Researchers developed machine learning systems analyzing sustained vowel sounds. Subtle irregularities in vocal fold vibrations indicated early neurological impairment.
Example Two: Wearable Monitoring
Smartwatches equipped with motion sensors detect tremor intensity and frequency. Data streams are analyzed in real-time to support neurologists.
Example Three: Handwriting Assessment
Patients drawing spirals on digital tablets reveal micro-motor impairments invisible to the naked eye. Algorithms classify patterns with high accuracy.
These real-world applications demonstrate how Detecting Parkinson’s Disease is moving beyond traditional clinical exams.
Machine Learning Models for Detecting Parkinson’s Disease
Several algorithms are commonly applied:
Logistic Regression
Used for binary classification problems.
Support Vector Machines
Effective in high-dimensional medical data.
Random Forest
Handles non-linear relationships well.
Artificial Neural Networks
Capture complex patterns in large datasets.
Deep Learning
Particularly effective for imaging data.
Each model undergoes training, validation, and testing to ensure clinical reliability.
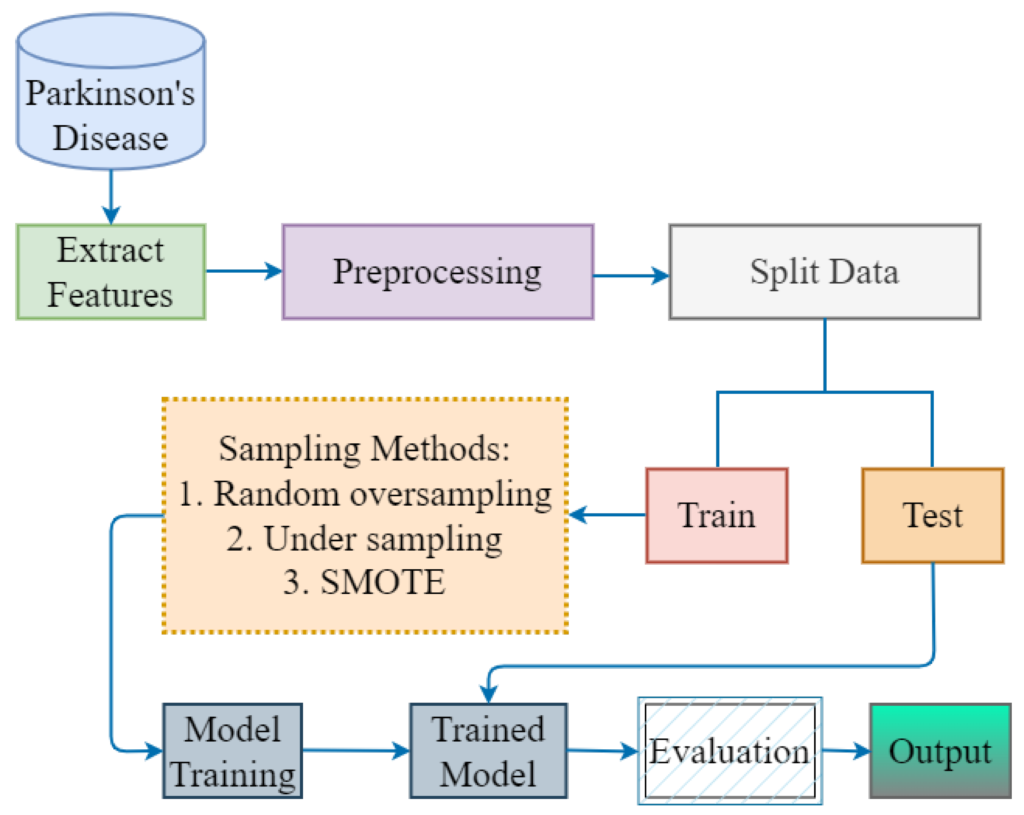
Feature Engineering and Data Preprocessing
Data preprocessing is critical for accurate predictions.
Steps include:
- Handling missing values
- Normalizing features
- Removing noise
- Balancing datasets
- Feature selection
Important voice features include:
- Jitter percentage
- Shimmer
- Harmonics-to-noise ratio
Feature engineering improves model accuracy and reduces overfitting.
Voice-Based Detection Systems
Voice impairment is one of the earliest symptoms.
AI systems extract acoustic parameters from recordings. These parameters are fed into classification models.
Studies show voice-based detection models achieve strong predictive performance in controlled settings.
Wearable Sensors and IoT Monitoring
Internet of Things devices continuously monitor:
- Tremor frequency
- Step count
- Gait symmetry
- Postural changes
Continuous monitoring provides longitudinal data, improving diagnostic confidence.
These technologies allow remote healthcare monitoring.
Medical Imaging and Computer Vision
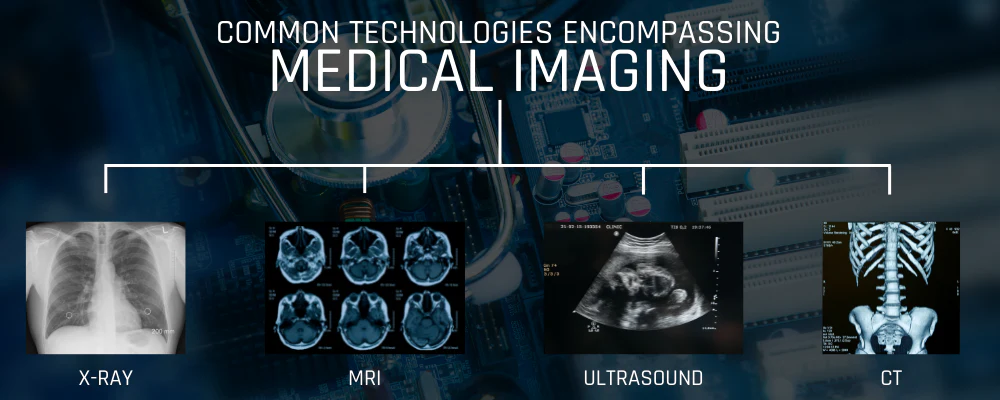
MRI and PET scans provide structural and functional brain information.
Deep learning models process imaging data using convolutional neural networks.
Computer vision techniques identify structural degeneration patterns.
Biomarkers in Detecting Parkinson’s Disease
While motor symptoms remain central to clinical diagnosis, emerging research highlights biological markers that can improve early-stage detection.
1. Alpha-Synuclein Aggregation
Alpha-synuclein protein accumulation in brain tissue is a hallmark of Parkinson’s disease. Recent laboratory techniques detect abnormal protein folding in cerebrospinal fluid samples.
Machine learning models can analyze biomarker concentration patterns to support early clinical decisions.
2. Dopamine Transporter Imaging
Dopamine transporter (DAT) scans measure dopamine activity in the brain.
Reduced uptake in specific brain regions indicates neurological degeneration.
Deep learning models trained on DAT scan datasets classify imaging results with high accuracy.
3. Genetic Markers
Certain gene mutations such as LRRK2 and SNCA increase Parkinson’s risk.
Genomic datasets combined with predictive modeling enable risk profiling for individuals with family history.
These biological signals strengthen multimodal approaches in Detecting Parkinson’s Disease.
Multimodal Learning for Parkinson’s Prediction
Single-source data often lacks sufficient predictive strength.
Multimodal AI combines:
- Voice features
- Gait sensor signals
- Imaging scans
- Genetic markers
- Clinical history
By integrating structured and unstructured data, neural networks capture more comprehensive patient profiles.
Example:
A hospital integrates wearable sensor data with MRI imaging results. The predictive model improves diagnostic confidence compared to isolated analysis.
Multimodal systems represent the future of neurological AI diagnostics.
Deep Learning Architectures Used in Detecting Parkinson’s Disease
Modern research applies advanced neural network structures.
Convolutional Neural Networks (CNNs)
Used primarily for MRI and brain scan analysis.
CNNs automatically extract spatial features from imaging data.
Recurrent Neural Networks (RNNs)
Applied to time-series data such as tremor signals and voice recordings.
They capture sequential dependencies in patient movement patterns.
Long Short-Term Memory Networks (LSTMs)
Particularly effective in analyzing gait signals over extended periods.
Transformer Models
Emerging research explores transformer-based architectures for biomedical signal processing.
These architectures enhance predictive performance in Detecting Parkinson’s Disease by learning complex nonlinear relationships.
Real-World Implementation Case Studies
Case Study: AI-Based Voice Screening Tool
A telemedicine startup developed a smartphone app that records short speech samples.
The AI model extracts:
- Fundamental frequency variation
- Vocal tremor
- Signal-to-noise ratio
Results are compared against trained classification models.
Clinical trials demonstrated strong sensitivity in identifying early vocal impairments.
Case Study: Hospital-Based Imaging System
A neurology department implemented a CNN-based MRI classification system.
The system reduced diagnostic time and improved standardization across clinicians.
AI assistance increased early-stage detection rates.
Data Imbalance and Model Optimization
Medical datasets often suffer from imbalance.
For example:
- Fewer early-stage cases
- Limited longitudinal records
- Small control group samples
To address this:
- SMOTE (Synthetic Minority Over-sampling Technique) generates synthetic samples.
- Cross-validation ensures robust performance.
- Ensemble learning improves generalization.
Hyperparameter tuning using grid search or Bayesian optimization further enhances performance.
Optimized models strengthen the reliability of Detecting Parkinson’s Disease systems.
Model Evaluation Metrics
Healthcare AI requires rigorous evaluation.
Common metrics include:
- Accuracy
- Precision
- Recall
- F1 Score
- ROC-AUC
In medical diagnosis, recall (sensitivity) is especially important because missing a positive case has serious consequences.
Confusion matrices help clinicians understand false positives and false negatives.
High-quality evaluation builds trust in predictive systems.
Regulatory and Clinical Validation
Before clinical deployment, AI systems must comply with medical regulations.
Important aspects include:
- Clinical trials
- Peer-reviewed validation
- Data privacy compliance
- Transparency requirements
In many countries, regulatory approval is required before AI systems can assist in medical diagnosis.
Model explainability tools such as SHAP values provide interpretability.
Transparent AI increases clinician adoption.
Role of Explainable AI in Neurology
Medical professionals require understandable outputs.
Explainable AI provides:
- Feature importance scores
- Visual attention maps for MRI
- Decision pathway summaries
Example:
A neurologist reviewing AI output sees that voice jitter and tremor amplitude were key predictive factors.
This transparency increases clinical confidence.
Federated Learning in Healthcare
Data sharing across hospitals is challenging due to privacy regulations.
Federated learning enables:
- Model training across institutions
- No raw patient data exchange
- Secure collaborative learning
This approach increases dataset size while preserving confidentiality.
It significantly improves model robustness in Detecting Parkinson’s Disease research.
Edge AI and Real-Time Monitoring
With wearable devices becoming common, edge AI processes data locally.
Advantages:
- Faster response time
- Reduced cloud dependency
- Enhanced privacy
Smart devices can alert patients and clinicians if tremor intensity exceeds baseline thresholds.
Continuous monitoring supports proactive intervention.
Economic Impact of Early Detection
Early identification reduces:
- Hospital admissions
- Advanced-stage treatment costs
- Long-term disability expenses
Healthcare systems benefit from:
- Reduced burden
- Improved patient independence
- Optimized treatment planning
Predictive analytics contributes to cost-effective healthcare management.
Integration with Telemedicine
Telemedicine platforms increasingly incorporate AI-driven screening.
Patients can:
- Submit voice samples
- Perform guided motor tests
- Upload wearable data
Remote neurological assessment expands access to underserved regions.
AI-based Detecting Parkinson’s Disease tools enhance telehealth services.
Comparative Analysis with Traditional Diagnosis
Traditional Diagnosis:
- Based on physical examination
- Relies on visible motor symptoms
- Subjective interpretation
AI-Based Diagnosis:
- Data-driven
- Identifies subtle patterns
- Continuous monitoring possible
- Quantitative and standardized
AI does not replace neurologists but augments decision-making.
Research Trends and Academic Contributions
Leading universities and medical institutions actively publish research on Parkinson’s prediction.
Research focuses on:
- Voice biomarker modeling
- Deep learning for MRI classification
- Digital phenotyping
- Wearable device analytics
Open-source datasets accelerate innovation.
Collaborative research strengthens scientific validation.
Practical Project Idea for Data Scientists
If you are writing for a technical audience, you can include this real-time project workflow:
Project Workflow:
- Load Parkinson’s dataset from UCI repository
- Perform exploratory data analysis
- Apply feature scaling
- Train multiple classifiers
- Evaluate using ROC-AUC
- Optimize hyperparameters
- Deploy using Flask or Streamlit
This hands-on example makes Detecting Parkinson’s Disease more practical for learners.
Ethical Risk Mitigation Strategies
To reduce bias:
- Use diverse datasets
- Audit model predictions
- Include cross-demographic validation
Healthcare AI must prioritize fairness.
Bias mitigation strengthens reliability across populations.
Future Innovations in Detecting Parkinson’s Disease
Future developments may include:
- AI-driven drug response prediction
- Brain-computer interfaces
- Advanced neuroimaging analytics
- Digital twin modeling for personalized treatment
As computational power increases, predictive accuracy will continue improving.
AI will become an integrated component of neurological healthcare systems.
Challenges in Detecting Parkinson’s Disease
Despite advancements, challenges remain:
- Small datasets
- Data privacy concerns
- Model interpretability
- Clinical validation requirements
- Regulatory approvals
Healthcare AI must prioritize transparency and explainability.
Ethical and Clinical Considerations
Ethical challenges include:
- Patient consent
- Algorithm bias
- Data security
- Over-reliance on automation
AI systems should support, not replace, neurologists.
Internal Linking Opportunities
You may link this blog to related articles such as:
- Machine Learning in Healthcare
- Supervised Learning Algorithms Explained
- Python for Medical Data Analysis
- Feature Engineering Techniques in Data Science
This strengthens SEO structure and improves engagement.
Future of AI in Neurological Diagnosis
The future includes:
- Multi-modal data integration
- Real-time remote diagnostics
- Personalized treatment recommendations
- Cloud-based healthcare analytics
Advancements in AI research continue to refine Detecting Parkinson’s Disease models for earlier and more reliable predictions.
Emerging technologies like federated learning may allow hospitals to collaborate without sharing raw patient data.
Conclusion
Neurological healthcare is entering a new era driven by predictive analytics and artificial intelligence. Early and accurate identification of motor and non-motor symptoms plays a critical role in improving patient outcomes.
Detecting Parkinson’s Disease using machine learning, wearable devices, and voice analytics is no longer experimental. It is rapidly becoming a clinical reality.
With continued research, ethical deployment, and cross-disciplinary collaboration, AI-driven diagnosis will significantly transform neurological healthcare.
FAQ’s
What are the first signs of Parkinson’s?
Early signs of Parkinson’s disease often include slight tremors, slowed movement (bradykinesia), muscle stiffness, and changes in handwriting or balance, which may gradually worsen over time.
How to detect Parkinson’s disease?
Parkinson’s disease is detected through clinical evaluation of motor symptoms (tremor, rigidity, slowed movement), neurological examination, medical history, and sometimes brain imaging tests to rule out other conditions.
What does Parkinson’s feel like?
Parkinson’s can feel like persistent stiffness, slowed movements, tremors, fatigue, and difficulty with balance or coordination, often progressing gradually over time.
What is a red flag for Parkinson’s?
A key red flag for Parkinson’s is a resting tremor in one hand along with slowed movements (bradykinesia) and muscle rigidity, especially if symptoms progressively worsen over time.
What is the finger test for Parkinson’s?
The finger test (often the finger-tapping test) assesses how quickly and smoothly a person can tap their thumb and index finger together; slowness, reduced amplitude, or irregular rhythm may indicate bradykinesia, a common sign of Parkinson’s disease.